Quarterly Provider Verification
The Consolidated Appropriations Act (CAA), also known as the “No Surprises Act”, will bring some changes for Blue Cross and Blue Shield of Vermont providers. These federal regulations requires us to work with our providers to verify the demographic information we have on file for their practice and each provider associated with their practice. The demographic information feeds into our provider directory for members.
Every 90 days, you will receive an email as part of this verification process. You are required to take the needed action, which can be completed in just a few steps as outlined below. We appreciate your ongoing attention to this verification process.
Completing the Provider Verification
Using the link provided in the email you received from Blue Cross for the quarterly provider verification, review the provider specific information contained on the form. Only providers at the practice who are marketed in our online provider directory will show on the form.
The demographic elements requiring verification are:
- Name – name of provider (first, middle, last); middle name is not required
- Taxonomy Code– the taxonomy number(s) used by the provider to identify their specialty
- Provider Specialty – the licensed specialty of the provider
- Address(es) – each physical location the provider is available to patients at
- Provider Phone – the phone number of each location the provider is located where patients can call to schedule appointments or speak with the provider
- Accepting Patients – Primary Care Providers need to validate their panel status. Specialists will always reflect an open patient panel
- Digital Contact – URL of practice web address, if available
- Hospital Affiliations – the hospital(s) a provider has admitting privileges to
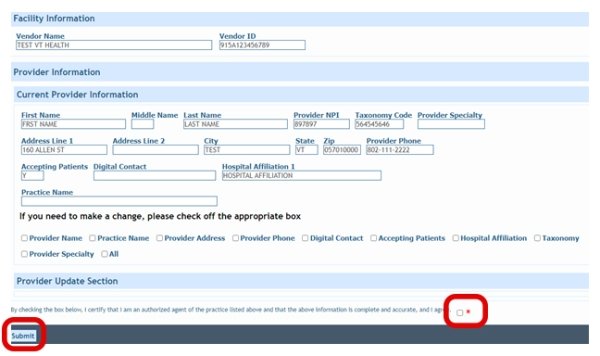
If all the information on your form is correct, simply click on the agree area in the Provider Update Section at the bottom of the form then submit (see below image below). No other action is required.
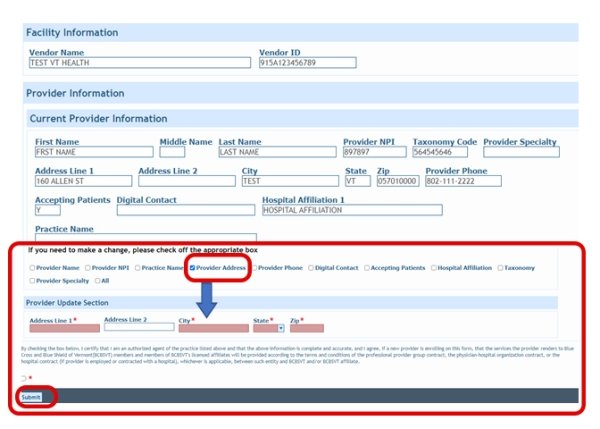
If information on your form needs to be corrected, go to the area of the form marked “If you need to make a change, please check off the appropriate box”. Click on the fields that need to be updated. When you check off each field, another section will expand for you to enter the correct information.
You will be required to attach additional documentation before submitting the form for the following scenarios:
- If this is a practice name change, you are also required to attach an updated W9. When practice name is checked, a box will display where you can attach the W9.
- If this is a provider name change, you are required to attach an update license. When provider name change is checked, a box will display where you can attach the license.
The image below shows a provider address checked to make an update. Fields with a red asterisk must be completed. Once you are done, check the box, certifying you are an authorized agent and submit. No other action is required.
Q: Why is Blue Cross requiring verification of provider directory information?
A: There are a couple of reasons:
- Maintaining accurate provider information is critically important to ensuring our provider directories are up to date and our members are able to access care with ease.
- The Consolidated Appropriations Act (CAA) mandates this verification process and we also must perform this verification to maintain National Committee for Quality Assurance accreditation.
Q: How frequently is provider verification required?
A: We will send out requests for provider verification quarterly: January, April, July and October. The first request was sent in October/November 2021.
Q: How is provider verification sent out?
A: We will send an email to the provider enrollment contact email supplied to us during initial enrollment, or the updated contact information if you have since updated the email address. The email is sent out by noreply@bcbsvt.com, so you will not have the ability to reply to this email. Please make sure you have provided appropriate security for this email address, so these emails are received into your inbox and are not moved to a “spam/junk” folder.
If you need to update your provider enrollment email address, please email the update to providerfiles@bcbsvt.com. Make sure to include your group NPI(s) to which the new email is applicable.
Q: How do I complete provider verification?
A: The email will contain a link to your practice information/provider(s) which will allow you to accept or change the reported data. There are some changes that will require additional information. For example, if a provider has had a name change, we will need a copy of the license with the providers new/updated name.
Q: If I have questions about the provider verification or need assistance who do I contact?
A: If your question is about the process or you have technical difficulties, you can contact Provider Relations either by email at providerrelations@bcbsvt.com or phone at (888) 449-0443 option 1. If you have questions about the details related to the providers in the link, you will need to contact Provider Files either by email at providerfiles@bcbsvt.com or phone at (888) 449-0443 option 2.
Q: How quickly do I need to act upon the provider verification?
A: As quickly as possible, but within 30 days would be appreciated. The link in the email is set to expire after a set time. If you do not respond to the email in a timely manner, you risk removal of your practice information/provider information from our provider directory.
Q: What elements require verification:
A: These are elements that require verification (see additional details above in the Instructions section)
- Name
- Taxonomy Code
- Provider Specialty
- Address(es)
- Provider Phone
- Accepting Patients
- Digital Contact
- Hospital Affiliations
Q: What happens if I do not verify the provider information, or am not timely in verifying?
A: If a timely verification is not completed, the providers will be removed from our online provider directory (also referred to as our Find a Doctor tool).
Q: If my provider(s) are removed from the online provider directory, how do I get them back in?
A: Once a quarterly update is completed, providers will be added back. For example, if you miss the January verification but verify in April, your providers will be added back upon receipt of the April verification.
Q: If my providers are removed from the online provider directory, will claims still process against my contract and will your customer service teams still be able to advise patients of my contracted status?
A: The impact will be to the online provider directory only. Claims will still process against your active contracts and our customer service teams will be able to advise as to your network status.
Q: If I identify incorrect information and update in the link, how long will it take to process and show?
A: Approximately five business days, unless additional paperwork is required to make the change.
Contact Us for Assistance
Have Questions or Need Assistance?
Connect with our team - we are here to help!
