Blue Cross Blue Shield of Vermont to Cover Certain Take Home Rapid COVID Tests

Blue Cross and Blue Shield of Vermont members can receive reimbursement for the costs of at home COVID-19 tests. Coverage for OTC COVID-19 tests is effective through the end of the Federal state of emergency.
UPDATE: April 2023
The Public Health Emergency ends for COVID-19 on May 11, 2023. We are here to help with the transition and help you understand what it means for your coverage of COVID-19 tests, vaccines and therapeutics and telehealth.
Changes to coverage of at-home COVID-19 tests will go into effect on July 1, 2023. Learn more about the changes on our COVID-19 Resources page.
UPDATED: September 2022
New Regulations for Plan Coverage of At-Home COVID Testing
Following federal regulations regarding the coverage of over the counter (OTC) COVID-19 tests, beginning January 15, 2022, members can receive reimbursement for the costs of at home COVID-19 tests. Coverage for OTC COVID-19 tests is effective through the end of the Federal state of emergency.
For more information about coverage for testing, as well as more updates and resources on COVID-19, visit our COVID-19 Updates page.
Instructions for seeking reimbursement for at-home tests purchased are listed below.
Vermont Blue Rx Pharmacy Coverage
- Members who have pharmacy benefits through Vermont Blue Rx can go to their local, in-network pharmacy, present their member ID Card, and request a take home rapid COVID-19 test covered under the pharmacy benefit. We encourage you to go through the pharmacy when possible as it is no cost to you and doesn’t require seeking reimbursement.
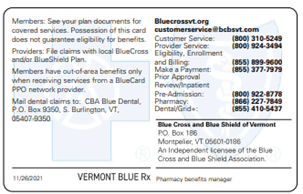
Not sure if you have Vermont Blue Rx pharmacy coverage? Your ID card can help! If you have this coverage, your member ID card will have the Vermont Blue Rx logo on the back. - There is a limit of eight tests per member, per 30-day period.
Reimbursement Process (beginning 01/15/2022)
If you purchased a COVID-19 test on or after January 15, 2022, and are seeking reimbursement, you’ll need to complete the steps below. There is a limit of eight tests per member, per 30-day period.
If you are seeking reimbursement for tests purchased between December 1, 2021—January 14, 2022, you will also follow the instructions below, with the exception of using a different Procedure Code (see notes below).
Members with Coverage Through Their Employer
If you have coverage through your employer and do not have Vermont Blue Rx pharmacy coverage, your employer may have a preferred pharmacy established for you to receive the at-home testing coverage benefit. Contact your employer for more information about how to receive reimbursement for at-home COVID-19 coverage options.
- Complete the Member Medical Claim Form using the following information:
- Provider Information: Include the name and address of the store, vendor, or practice that sold you the test.
- Description of Service: COVID-19 Rapid At-Home Test
- Procedure Code (for tests purchased on/after 01/15/2022): S1002*
- *For tests purchased between 12/01/2021—01/14/2022, use Procedure Code 87426
- *Federal Employee Program (FEP) members must use a different code for reimbursement. Contact the FEP customer service team for assistance.
- Diagnosis code: Z20.822
- Charge: For tests purchased on/after February 4, 2022, list the amount paid including any additional charges such as tax, postage, or shipping and handling. If you are seeking reimbursement for tests purchased prior to February 4, 2022, only include the amount paid and exclude any additional charges.
- Units (Tests): We cover up to eight tests per member, per 30-day period. One test equals one unit.
- POS: 12
- While members can submit a claim using fax or mail, the quickest and easiest method is to submit through the Member Resource Center, following the instructions on top of the claim form.
- Finally, don’t forget to include a copy of your receipt with the claim form. If tests were purchased for multiple family members on a single receipt, please indicate on the receipt how many tests were purchased for each family member (i.e. Suzie (3) and Bill (4)). This helps ensure the submitted claim aligns with the receipt.
Covered Tests
All over the counter rapid tests that have Emergency Use Authorization (EUA) from the Food and Drug Administration (FDA) are covered under the federal regulation (antigen and LAMP tests). We will reimburse members for rapid COVID-19 tests listed on the FDA’s OTC approved list (please note: the lists are subject to change at this link) which are taken and read for results at home. Tests that are taken at home but sent to the lab for processing are not eligible for reimbursement at this time.
Tests that are purchased for return-to-work will not be covered per the federal regulations.
Original News Release: December 8, 2021
Berlin, Vermont — Vermonters who receive their pharmacy benefit through Blue Cross and Blue Shield of Vermont (Blue Cross) will have coverage for certain FDA-authorized take home rapid COVID-19 tests beginning in December. As cases rise to alarming levels in our state, we need to use every tool at our disposal to stem the spread of COVID-19 in our communities. At-home testing is just one component and must be part of a suite of health precautions to keep our families and community safe this winter.
Take-home rapid COVID-19 tests will be covered with a prescription from a provider or pharmacist. There is a limit on the number tests per person per month. Because of a shortage of tests nationally and difficulties for pharmacies in procuring the appropriate tests, we strongly encourage Vermonters to avoid stockpiling. All FDA-Approved test kits in the Medispan database will be covered through our member’s pharmacy benefit without any individual cost-share.
We join our Vermont health care partners in encouraging our neighbors to redouble their COVID precautions. Our hospitals are nearing capacity and ICUs are struggling to meet the demand of patients with high acuity while at the same time treating the high number of critical COVID cases. We must remain vigilant, despite our exhaustion with the pandemic. Please:
- Wear a mask when indoors in public places, and outdoors when you are unable to social distance, and wash hands often.
- Get vaccinated if you are not already and boosted as soon as you are able. Encourage your friends and loved ones to join you.
- Stay home when you or your children are experiencing symptoms, and while awaiting test results. If your children are involved in a childcare or after-school program, remind them of your expectation around COVID precautions.
These safeguards will not only stem the spread of COVID, it will also keep your family, your parents, your friends, and your community safe as we fight this terrible disease together.
How to get a free take home rapid COVID-19 test
Members who have pharmacy benefits through Vermont Blue Rx can go to their local, in-network pharmacy, present their member ID card, and request a take home rapid COVID-19 test covered under the pharmacy benefit. When purchasing tests, you’ll want to show the member ID card for each family member you’re purchasing a test for.
For take home rapid COVID-19 tests purchased in December 2021, there is a limit of 16 tests per month, per member. As many testing kits include 2 tests per package, this is generally 8 testing kits. Due to limited supply, some pharmacies may not have covered tests in stock. In this case, you will be asked to pay out of pocket and submit a reimbursement claim.
Members who purchased a test kit prior in December 2021, those out of the state of Vermont, or don’t have pharmacy coverage through Vermont Blue Rx, may also submit a claim for reimbursement. Coverage can vary for members covered through their employer. We encourage you to check with your employer to verify if your plan will cover the rapid at home tests.



